You must log in or register to comment.
United’s response, according to communications I got as a provider, is to drop reimbursement for mental health providers in the optum network starting in January
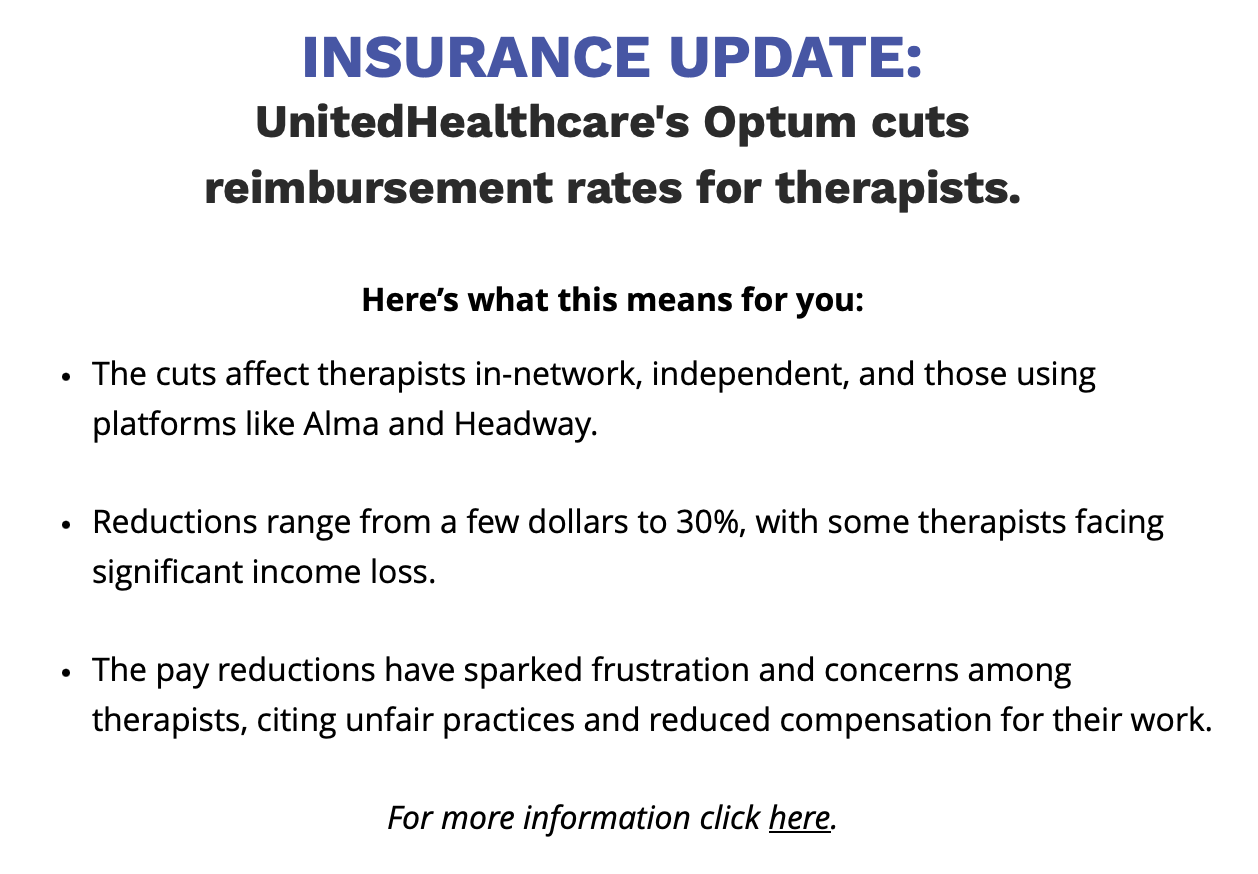
What this means is more therapists will either make even less money or simply drop optum from their paneling, meaning clients with that insurance will have less options for treatment providers (or will need to use out of network benefits, which are a pain in the ass and much easier for insurers to deny).
This communication came from mentaya, a company that makes its money by “helping people to navigate out of network benefits”, eg they see this as a business opportunity
What a bizarre headline. He had a prison makeover? Anyway, death to Daily Beast.



